In order to effectively train Soldiers to feel comfortable providing medical care to females, and to react without hesitation in life-threatening situations, trainees should be given the opportunity to train with realistic female anatomical models and be exposed to female severe trauma injury patterns observed at the point of injury.
This paper will highlight relevant female casualty research and current efforts to develop multiple solutions to fill this training gap. Specific to this paper, the research will discuss the literature on female simulation, provide anecdotal evidence of the training gap, and explain current trends highlighting the need for female simulation. It is expected that results from this research will translate into a more comprehensive training experience for all service members.
Background
Pre-hospital care plays a vital role in battlefield medicine. Tactical Combat Casualty Care (TC3) principles have become the standard of care on the battlefield establishing when and how much care can be provided based on the tactical situation. These principles have proven highly effective and resulted in lower mortality rates (Butler, 2010).
In March 2015, the US Department of Defense (DoD) Defense Health Board (DHB) published a report on Combat Trauma Lessons Learned from Military Operations of 2001-2013, documenting findings from the conflicts in Iraq and Afghanistan. The report acknowledges that the survival rate of Service members injured in combat has significantly improved due to advances in trauma care and knowledge gained by military medical personnel in the pre-hospital, far-forward environment (Defense Health Board [DHB], 2015).
The DHB committee emphasized that trauma training should be integrated into operational and tactical training, and include training exercises that are emotionally demanding, physically intense and realistic. Scenario-based exercises must include basic critical tasks and focus on mastery of skills, not merely familiarization. Therefore, military medical personnel must be trained in a realistically accurate combat environment to ensure they have the necessary decision-making and teamwork skills to treat the wounded effectively (Lateef, 2010). An effective method includes SBT, which plays a major role in the development of psychomotor skills necessary to treat severe trauma on the battlefield. Further, SBT paired with existing training coursework provides an effective teaching method (Beal, Kinnear, Anderson, Martin, Wamboldt, and Hooper, 2017) based on the user’s education or instructional goals (Kim, Park, and Shin, 2016).
The primary mission of military medical personnel is to treat the wounded and save lives. First responders (also known as Combat Medics or Combat Life Savers) are responsible for providing the first line of medical care to casualties at the point of injury. Data from the theater show that the majority of casualties who die in combat do so before reaching a definitive care facility (Eastridge, et al., 2012). Therefore, decisions made and the treatments applied during pre-hospital care directly impact the survivability of the casualty. Severe trauma produces major challenges to front line medical providers because many are not mentally, psychologically, or technically prepared to treat such emotionally disturbing wounds. Soldiers treating such wounds must be trained in a realistically accurate combat environment to ensure they have the necessary skills to effectively treat casualties.
According to the Deputy Director of the Department of Combat Medic Training at Fort Sam Houston TX, Mr. Donald Parsons remarks:
Trauma simulation needs to be realistic. Students should have the ability to practice life-saving interventions on a realistic manikin to develop skills and confidence. The first time they have to care for a casualty with bilateral amputations should not be on a real person. Having treated similar wounds on a simulator gives them a little picture in the back of their mind that they have done this before, successfully, and they now have the confidence to perform. (Feb 2016)
Military medical personnel must be trained in a realistic and accurate combat environment to ensure they have the necessary skills to treat the wounded effectively. Current research should focus on developing the most realistic, physiologically based, and cost effective simulation technologies in order to give our Soldiers the most realism possible to support stress inoculation training.
Stress inoculation, also referred to as desensitization, is needed during training to reduce the emotional reaction or shock the medic experiences in response to blast trauma at the point of injury in operational environments. Such reactions may cause the medic to hesitate or otherwise interfere with his/her performance in saving lives through prompt and effective medical response. An inexperienced medic’s natural response, when facing these traumatic injuries for the first time, is a reluctance to treat the casualty. The negative effect on performance associated with dealing with such disturbing wounds can directly impact the survivability of the injured.
Trauma training should incorporate gender specific differences to allow first responders to practice their critical thinking skills and build muscle memory. Simulating injury patterns that take into consideration female anatomical and physiological differences provide opportunities to psychologically prepare Soldiers to deal with the challenges posed by these types of injuries. Providing operationally relevant training scenarios allow soldiers to develop critical thinking and psychomotor skills within the context of situations that they might encounter in theater.
Current human patient simulation models used to train first responders are decidedly masculine in appearance. Female simulation is unrealistic, and frequently a mere adjunct to the male-centric training device. Capabilities in the training environment should incorporate realistic female anatomy and severe trauma injury patterns in order to make both male and female Soldiers more comfortable with providing care to females and reduce the sensitivity to their anatomy.
Critically, in addition to these considerations, any potential training solution must be rugged enough to endure thousands of uses per year, require minimal logistical support, and be cost-effective. This presents an engineering challenge to develop more effective and realistic training systems, at the appropriate level of fidelity, while supporting specific training objectives in a limited resource environment.
How do gender differences impact the training environment?
Modern medicine has become more aware of the anatomical and physiological differences between men and women, aside from just reproductive systems. And it’s really looking at what that means for emergency medicine, particularly for health outcomes.
These differences are not reflected in the training literature. For example, in the Prehospital Trauma Life Support (PHTLS) military manual, developed by the National Association of Emergency Medical Technicians (NAEMT) in the early 1980s in cooperation with the American College of Surgeons Committee on Trauma (ACS-COT), female casualties are underrepresented. Female representation made up only approximately 24% of graphics depicting casualties or procedures (72 females and 237 males) and there is no discussion of physiological variation between genders (Prehospital Trauma Life Support [PHTLS], 2014).
Through Practice
Anecdotal data gathered from a previously deployed Combat Medic in the United States Army provides a poignant example of the impact of gender differences in battlefield medicine, and the need for action:


“I treated a female with a full amputation right arm above the elbow at Point Of Injury in Iraq. I pulled out my SOFTT and began applying it to the stump. After I began to tighten the tourniquet, I realized that the windlass would not secure due to the fact that her arms were small. I had to have her hold the windlass while I applied a CAT tourniquet above the SOFTT. After this incidence I began training my medics differently and also changed the way I did medicine. Women are built differently, their joints are smaller and typically they have a smaller frame. This is a common fact that we must address to ensure we are providing the safest life-saving measures available.”
Through Survivability Rates
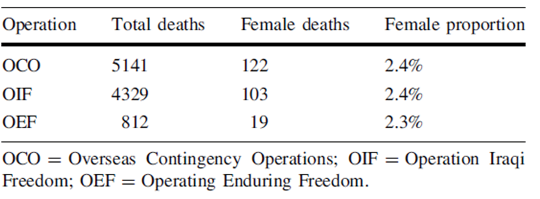
A literature review revealed critical information in regards to survivability differences between male and female in a combat environment. According to Cross, et al. (2011), data from the Joint Theatre Trauma Registry dating from 2001 to 2009 (Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) showed that battle-injured females had a lower survivability rate compared to their male counterparts (OEF 35.9% vs 17%; OIF 14.5% vs 12%). A significant proportion of female casualties’ injuries were located in the abdominal and chest region, compared to their male counterparts who survived. One plausible explanation is that the higher death rate of females may be a result of them encountering explosives during supporting roles, rather than a result of gunshot wounds where body armor is worn (Cross, et al., 2011). The following table illustrates the proportion of females’ death compared to female casualties.
Additionally, Belmont et al. (2010), conducted a 15 month study to determine combat casualties and injuries of Soldiers deployed in Iraq. Females consisted of a smaller population percentage (7.9%), while accounting for 12.5% of Disease Nonbattle Injuries (DNBI). Females had a significantly higher incidence rate of 408.6 per 1,000 combat years, in comparison to males’ 244.0 per 1,000 combat years. Females had significantly higher rates for being a DNBI casualty requiring MEDEVAC. Thirty-five of the 325 females that required MEDEVAC were due to reproductive issues. Overall, the results indicated that 75% more Soldiers were lost due to DNBI than combat casualties in the battlefield (Belmont, Goodman, Waterman, DeZee, Burks, and Owens, 2010). As of August 2018, survivability rates still show lower numbers for female casualties (OIF: 14.9% vs 12.1%; OEF: 11.5% vs 10.5%; Operation Freedom’s Sentinel (OFS) 25% vs 14%) (Defense Manpower Data Center [DMDC], 2018).
Survival rates for casualties have improved over the past century, from 80% in World War II, to 84% in Vietnam, to an unprecedented historical level of 90% in Iraq and Afghanistan. However, 18% of deaths on the battlefield are preventable by proper medical interventions. A recent review (2001 to 2011) identified exsanguination as the number one leading cause of preventable death followed by airway obstruction and tension pneumothorax (Eastridge, et al., 2012). In a study of sucking chest wounds and other traumatic chest injuries, data showed that when assessed by gender, the needle chest decompression (NCD) procedure, which is used to relieve a tension pneumothorax, had a higher success rate in males than females (Inaba, Branco, Eckstein, Shatz, Martin, Green, Noguchi, & Demetriades, 2011). This could be attributed to anatomical differences between males and females. Sanchez, et al. (2011), reported that when considering gender differences in a civilian environment, women had shorter distances from skin to pleura compared to men. On the other hand, a study conducted in a military trauma center (Givens, Ayotte, & Manifold, 2004) showed that on average, women had thicker chest walls compared to male counterparts.
Through Anatomical Differences
In regards to physiological differences, research from civilian medical studies have concluded that hormonally active women benefit from their estrogen powering immune system (Frink, Pape, van Griensven, Krettek, Chaudry, & Hildebrand, 2007), have a better physiologic (hemodynamic and tissue perfusion) response to similar degrees of shock and trauma than their male counterparts (Deitch, Livingston, Lavery, Monaghan, Bongu, & Machiedo, 2007); and demonstrate a higher survival rate than males with comparable injury (Cross, et al., 2011). These results seem contradictory to what we are observing at point of injury (combat environment) where females are far more likely to die of their wounds than males. As a result, the authors surmise that at the point of injury, during which a male emergency care provider might be required to expose and/or touch a female Soldier’s body parts, lack of proper training can induce hesitation, which could potentially compromise the chance of performing a thorough assessment of injuries and jeopardize saving a critically injured female Soldier.
A Growing Trend
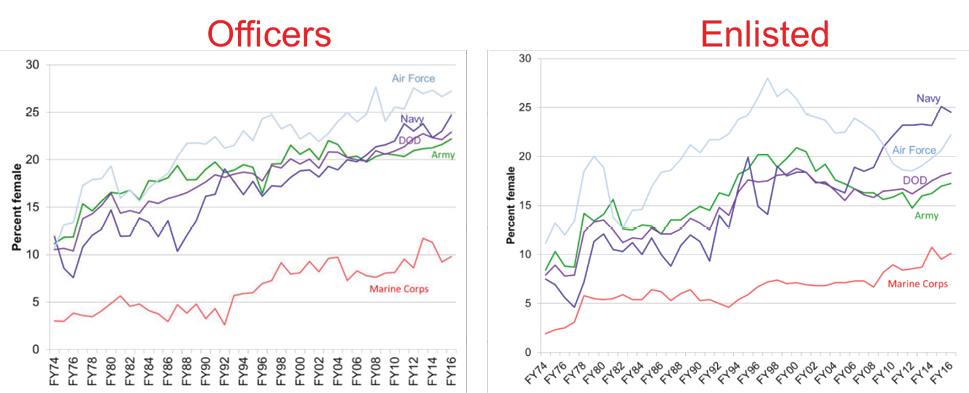
Recent studies have highlighted a need to explore the impact of sex and gender in clinical training to improve outcomes for female patients (McGregor and Choo, 2015). Following Defense Secretary Leon Panetta’s decision to lift the ban of women serving in combat arms in 2013, the number of females in combat roles is projected to increase drastically in the next few years (Hylden, Johnson, and Rivera, 2014; Office of the Undersecretary of Defense, Personnel and Readiness [OUSD(P&R)], 2016).
Within two years of Army recruitment, more than 640 women entered previously closed Infantry, Field Artillery, Ordnance and Combat Engineer branches. Thought must also be given to the other branches of service as the Marine Corp recruited 236 women to fill previously closed infantry roles. With over 300,000 woman being deployed since September 11, 2001 to Iraq and Afghanistan; 166 killed in combat and over 1,000 wounded, this number is guaranteed to rise without proper desensitization training for the first responders. The number of women currently in the training pipeline is growing and as this female population catapults past 15% of the military population, medical training with gender specific training models must be at the forefront. (Service Women’s Action Network, 2017).
With the shift in combat roles, military training needs to be assessed. A former combat medic who deployed with 3rd Cavalry Regiment in 2010 believes that with the placement of females in combat roles as Infantry Soldiers there needs to be an adjustment of the way the medical field trains interventions and treatments. She explained that in Advanced Individual Training (AIT) she trained on male-centric mannequins and when the question was asked she said the response was “There are no males and females…there are only Soldiers.” She states, “If the military doesn’t think this approach will be reflected on the battlefield in medical care, they are wrong. Males do hesitate to treat females, even if only for a second, to contemplate the touching of a female. I have witnessed hesitation. I have been asked to step in and relieve a male treating a female Soldier. I have also been asked to see females for basic sick call functions because the male medics are uncomfortable.” She went on to say that “Leadership needs to understand that just because we have always trained a certain way doesn’t mean it is the best approach. Research needs to be done to ensure we provide the very best POI care to everyone.”
As female numbers continue to increase in combat roles, more research is needed to investigate biological differences (i.e., males vs. females), mechanisms of injury, and treatment plans. Further, psychosocial factors (e.g., differences in symptom reporting; Farace and Alves, 2000) and perceptual issues in regards to hesitation are also a matter of consideration.
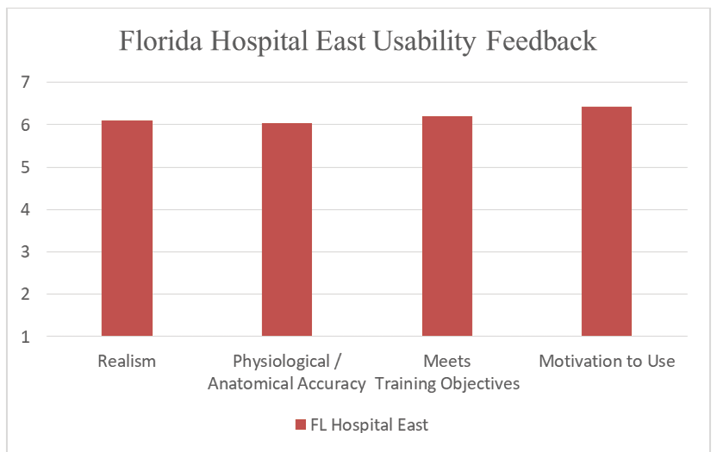
Table 2: Mean Responses by Category.
| Category | Response |
| Realism | 6.11 |
| Physiological/Anatomical Accuracy | 6.03 |
| Meets Training Objectives | 6.20 |
| Motivation to Use | 6.42 |
| All Categories | 6.19 |
This compilation of evidence points to the need for training programs to change. The examples of adjusting procedures to compensate for physical differences, the trend of lower survivability rates in major conflicts, and anatomical differences beneath the skin’s surface, combined with the rising proportion of female Soldiers, indicates that the Department of Defense could potentially face significantly diminished survivability in future conflicts. This evidence warrants a comprehensive analysis to determine the primary drivers impacting the survivability of female Soldiers. Results from such a study can inform programs of instruction on how best to incorporate gender differences during training. It is essential for the joint military community to eliminate gender as a variable with respect to survival at the point of injury, and throughout prolonged field care (PFC).
How is the US Army addressing the current training gap?
The US Army is currently conducting research and development of a female simulation model exhibiting high-fidelity anatomical and physiological structures. The targeted training audience are non-physician first responders. Specifically, current efforts focus on the development and evaluation of a low-cost female simulation-based model to support the training of Combat Lifesavers and Combat Medics in the development of psychomotor skills to treat severe trauma on female casualties at the point of injury.
The following is a list of required features identified by the military medical training community to support their programs of instruction. Any potential training solution must:
- Support established TC3 training objectives;
- Provide a capability to judge proficiency performance;
- Support practice of both cognitive and psychomotor skills;
- Include palpable anatomical landmarks to support the practice of TC3 procedures;
- Include realistic female simulated anatomical features to augment physical exam and scenario training; and
- Simulate female physiological responses; and
- Support training for long-term treatment during prolonged field care (PFC)
Currently, the Army is managing four efforts to develop a highly realistic female-centric simulation-based model. One of the efforts is focusing on developing a female model to interface with existing male-centric human patient simulation models. This capability will provide an immediate solution using current resources. The other three ongoing efforts are part of a Small Business Innovation Research (SBIR) topic to develop additional capabilities.
Initial Capability
One of the challenges in providing realistic human patient simulations is providing training models at the appropriate level of fidelity to cause stress inoculation, while also controlling costs. The DoD invests significant capital to acquire and maintain sophisticated human patient simulators (HPS) for point of injury training. Unfortunately, even these simulators do not meet the goals of realism and stress inoculation capability with respect to their female components.
Considering this significant investment, the Army decided to augment these already-existing HPS systems with more realistic anatomy with as little logistical footprint as possible by developing an interoperable add-on kit. This effort involved researching materials to obtain desired performance capabilities (e.g. self-healing skin that does not show holes from previous needle punctures), and increase the fidelity of female anatomical structures, while also greatly controlling costs.
The initial prototype consists of a torso and face overlays (as shown below in Figure 1) which interface with existing HPS systems used at the Army’s Medical Simulation and Training Centers (MSTCs).
A usability study was performed on the initial prototype on a noninterference basis with physicians from Florida Hospital East in Orlando, Florida (n = 22). This study focused on evaluating system usability to support training objectives and to assess if the system is intuitive, effective, and subjectively acceptable to users (Nielsen, 1993). Responses were obtained through a questionnaire that assessed the system with respect to benefit to training, usability, realism, physiological and anatomical accuracy, and motivation to use. Responses were reported using a 7-point Likert scale, with 7 indicating the most positive response. Initial usability testing indicated a strong level of user acceptance, as shown in Table 2 and Figure 2.
Based on the initial study findings, the system design was improved to incorporate a realistic face mask to slip on top of the existing face, as well as more realistic genitalia inserts to support catheterization training.
Successive usability testing continued to indicate a strong level of user acceptance using the same survey instrument. Feedback was obtained from a variety of potential end-users, including seven Combat Medics (68Ws) and 26 paramedics and EMTs (Mazzeo, Sotomayor, Coulter & Alban, 2018). On a 7-point Likert scale, 68Ws gave the system a score of 5.91, with 7 being the highest possible score. Physicians rated the system even more favorably at 6.19, while paramedics and EMTs rated it less favorably at 5.39.
This evaluation comprised a larger study population, as well as three different types of potential users. The original group consisted only of physicians from Florida Hospital East, whereas the successive groups consisted of a mix of combat medics, as well as paramedics and EMTs. These different groups might help explain the differences in reported scores for the system. An analysis of the data revealed the presence of a bimodal distribution of scores within the group of paramedics and EMTs from Estero Fire Rescue; roughly half of the participants reported a high level of acceptance, while the other half reported a low level of acceptance. This bifurcation explains the lower average score when compared to the first group’s usability data.
In addition to the usability data, several anecdotal observations were made during the course of this study involving 68Ws:
- Most trainees showed an initial pause when presented with the bra during patient assessment.
- Over half of the trainees did not remove the bra while assessing the patient.
- Most of the trainees that did remove the bra, spent time covering the breast or re-fastening the bra after the wound had been treated.
- One of the male trainees placed the occlusive dressing over the bra, making it ineffective. The instructor verbally told him that air was escaping from the dressing and he began to place a second dressing right on top of the previous one. The instructor used it as a teaching point that the occlusive dressing is only effective if it is placed on skin with no leaks. At that point the trainee moved the bra to the side and repositioned the dressing but still would not fully remove the bra. At this point the trainee was allowed to progress to the next training prompt.
- Overall, it appeared that the bra added another dimension of training and should be included in training scenarios moving forward.
- One participant seemed to struggle with counting the intercostal spaces. It is unclear if the overlay prevented proper palpation.
- One female participant approached the researchers after the simulation and stated that she really enjoyed using the female simulation system. She also mentioned that even as a female, she did not know what she was supposed to do in regards to the bra. She did not know if she was supposed to expose her or leave the bra on.
Over the course of the usability evaluation with the paramedics and EMTs from Estero Fire Rescue, several additional anecdotal observations were reported:
- Some participants removed the bra, but failed to properly assess the chest area.
- Out of 26 total participants, all but two failed to identify an injury close to the breast on the patient (a large bruise).
- Most participants felt that the face mask was not realistic enough to represent a female – it still appeared very masculine to them.
Through developing and testing a low-cost system to introduce female anatomy at an appropriate level of fidelity, not only did users find the system very usable, it also revealed a variety of potential psychomotor difficulties that would have been entirely absent without a realistic female model as part of the training regimen.
Future Capability
In addition to a rapidly deployable, low-cost training capability, the US Army is also investing in several additional capabilities through the Small Business Innovative Research (SBIR) Program. Three efforts are currently exploring how to incorporate female anatomy and physiology as it relates to combat trauma, under the topic entitled “Severe Trauma Female Simulation Training System.” The objective of this SBIR topic is to develop a realistic SBT system to support the development of psychomotor skills to treat severe trauma at point of injury. The capabilities developed under this SBIR will support not only the practice of cognitive and psychomotor skills, but also the ability to judge proficiency and performance through the use of software, sensing technologies, and physiology engines.
This research is ongoing, and initial capabilities will be available for assessment in FY2020. At that time, the direction of research will turn to evaluating the effectiveness of these capabilities in a relevant training environment. Concurrently, literature research will also be expanded to include additional data regarding male and female survivability rates with respect to battlefield injuries. The current survivability rates reported do not take into consideration factors such as the mechanism of injury, complications that arise as a result of injury, injury context with respect to roles (whether combat or non-combat roles), and differentiating between mortality as a result of combat and mortality as a result of non-battle related activities. For all of these factors, frequency and severity should be compared
Conclusion
Pre-hospital care plays a vital role in battlefield medicine. First responders must be trained in a realistic and accurate combat environment to ensure they have the necessary skills to treat the wounded effectively. Although women have typically been excluded from combat arms roles in the past, recently they have been represented in significant numbers in front-line positions. As aforementioned, following Defense Secretary Leon Panetta’s decision to lift the ban of women serving in combat arms in 2013, the number of females in combat roles is projected to increase in the next few years. In order to make male Soldiers more comfortable with providing care to female casualties, and more capable of reacting without hesitation in life-threatening situations, all trainees should be given the opportunity to train using realistic female anatomy models and be exposed to female severe trauma injury patterns prevalent at point of injury. The motivation behind this initiative is to provide Soldiers with the necessary tools and experiences in an immersive and realistic training environment to expose them to the realities of war including gender specific challenges.
References
- Beal, M. D., Kinnear, J., Anderson, C. R., Martin, T. D., Wamboldt, R., & Hooper, L. (2017). The Effectiveness of Medical Simulation in Teaching Medical Students Critical Care Medicine: A Systematic Review and Meta-Analysis. Simulation in Healthcare, 12(2), 104-116. doi:10.1097/sih.0000000000000189
- Belmont, J. P. J., Goodman, G. P., Waterman, B., DeZee, K., Burks, R., & Owens, B. D. (2010). Disease and Nonbattle Injuries Sustained by a U.S. Army Brigade Combat Team During Operation Iraqi Freedom. Military Medicine, 175(7), 469-476. doi:10.7205/MILMED-D-10-00041
- Butler, F. K. (2010). Tactical combat casualty care: update 2009. Journal of Trauma and Acute Care Surgery, 69(1), S10-S13.
- Cross, J. D., Johnson, A. E., Wenke, J. C., Bosse, M. J., & Ficke, J. R. (2011). Mortality in female war veterans of operations enduring freedom and Iraqi freedom. Clinical Orthopaedics and Related Research®, 469(7), 1956-1961.
- Deitch, E. A., Livingston, D. H., Lavery, R. F., Monaghan, S. F., Bongu, A., & Machiedo, G. W. (2007). Hormonally active women tolerate shock-trauma better than do men: a prospective study of over 4000 trauma patients. Annals of surgery, 246(3), 447-455.
- DHB report 150309 Defense Health Board Combat Trauma Lessons Learned from Military Operations of 2001-2013 March 9, 2015.
- Defense Manpower Data Center (DMDC) Defense Casualty Analysis System, retrieved August 7, 2018 from https://dcas.dmdc.osd.mil/dcas/pages/casualties.xhtml
- Eastridge, B. J., Mabry, R. L., Seguin, P., Cantrell, J., Tops, T., Uribe, P., … & Butler, F. K. (2012). Death on the battlefield (2001–2011): implications for the future of combat casualty care. Journal of trauma and acute care surgery, 73(6), S431-S437.
- Farace, E., & Alves, W. M. (2000). Do women fare worse: a metaanalysis of gender differences in traumatic brain injury outcome. Journal of Neurosurgery, 93(4), 539-545. doi:10.3171/jns.2000.93.4.0539
- Frink, M., Pape, H.-C., van Griensven, M., Krettek, C., Chaudry, I. H., & Hildebrand, F. (2007). Influence of sex and age on mods and cytokines after multiple injuries. Shock (Augusta, Ga.), 27(2), 151-156.
- Gilmore, W.S. (2013). Treating Sucking Chest Wounds and Other Traumatic Chest Injuries. Journal of Emergency Medical Services (Jul 19, 2013). Accessed at: http://www.jems.com/articles/print/volume-38/issue-8/patient-care/treating-sucking-chest-wounds-and-other.html
- Givens, M. L., Ayotte, K., & Manifold, C. (2004). Needle thoracostomy: implications of computed tomography chest wall thickness. Academic emergency medicine, 11(2), 211-213.
- Hylden, C., Johnson, A., & Rivera, J. (2014). Casualty sex differences: A new dilemma in modern warfare. American Academy of Orthopaedic Surgeons Now, 9(3).
- Inaba, K., Branco, B.C., Eckstein, M., Shatz, D. V., Martin, M. J., Green, D. J., Noguchi, T. T., & Demetriades, D. (2011). Optimal positioning for emergent needle thoracostomy: A cadaver-based study. J Trauma. 2011; 71(5):1099–1103.
- Kim, J., Park, J. H., & Shin, S. (2016). Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ, 16, 152. doi:10.1186/s12909-016-0672-7
- Lateef, F. (2010). Simulation-based learning: Just like the real thing. Journal of Emergencies, Trauma and Shock, Vol 3, Iss 4, Pp 348-352 (2010) (4), 348.
- Mazzeo, M. V., Sotomayor, T. M., Coulter, J. N., & Alban, A. M. (2018). Development & Assessment of a Human Patient Simulator Gender Retrofit Kit. Proceedings from the Interservice/Industry Training, Simulation, and Education Conference (I/ITSEC), Orlando, FL, November 2018.
- McGregor, A. J., & Choo, E. (2012). Gender-specific Medicine: Yesterday’s Neglect, Tomorrow’s Opportunities. Academic Emergency Medicine, 19(7), 861-865. doi:10.1111/j.1553- 2712.2012.01389.x
- Nielsen, J. (1993). Usability Engineering. Boston: Academic Press.
- Office of the Under Secretary of Defense, Personnel and Readiness Report, 2016. Retrieved August 7, 2018 from https://www.cna.org/pop-rep/2016/summary/summary.pdf
- Sanchez, L. D., Straszewski, S., Saghir, A., Khan, A., Horn, E., Fischer, C., & Camacho, M. A. (2011). Anterior versus lateral needle decompression of tension pneumothorax: comparison by computed tomography chest wall measurement. Academic Emergency Medicine, 18(10), 1022-1026.
- Office of the Under Secretary of Defense, Personnel and Readiness Report, 2016. Retrieved August 7, 2018 from https://www.cna.org/pop-ep/2016/summary/summary.pdf
- Service Women’s Action Network. (2017, 2 1). Women In International Security. Retrieved from Women in Ground Combat: Facts and Figures: https://www.servicewomen.org/wp-content/uploads/2017/02/Women-in-Ground-Combat-Arms-Fact-Sheet-2-1-17.pdf